Pulmonary Hypertension
July 2023
Author: Reena Sheth MD PGY3
Peer Reviewers: Joseph Babinski MD PGY2, Matthew Villanyi MD PGY4, Michael Campbell MD PGY3, Michael DeFilippo DO PGY4, Shriman Balasubramanian DO PGY3
Faculty Editor: Angela Barskaya MD, Assistant Professor of Emergency Medicine and Critical Care at Columbia University Medical Center
Case
A 66 year old female presents to the ED for shortness of breath. She has had a productive cough for the past 3 days, and today has a fever.
PMH: Sjogren’s related ILD c/b severe pulmonary HTN (class I/III) and R heart failure for which she is on continuous treprostinil via SQ pump and has a baseline O2 requirement of 6L/min
Vitals: BP 108/86 mm Hg; HR 118 bpm; RR 39/min; SpO2 89% on 6L/min NC; T 38.2ºC
Physical exam:
Gen: alert, sitting upright in respiratory distress.
CV: tachycardia, regular rhythm
Pulm: tachypnea, accessory muscle usage, diffuse fine crackles b/l, no rales or wheezing.
Abd: soft, nontender. Implantable pump for treprostinil infusion in place.
Ext: 1+ pitting edema of b/l LE
POCUS:
Lungs: mild scattered B-lines, +lung sliding b/l, some consolidation of LLL
Heart: dilated and hypertrophic RV with flattening of the interventricular septum
IVC: 2cm, minimal respiratory variation
How do we approach this patient? It would make sense to jump right in to resuscitation– she’s obviously on the brink of respiratory failure and you wouldn’t be wrong to get started without waiting for more data. But, it is important to recognize that this patient’s underlying pathophysiology is unique and ultimately some of our standard practices (i.e. NIPPV, intubation) may cause further decompensation.
First, the basics. Pulmonary hypertension is defined as an elevated mean pulmonary arterial pressure ≥25 mmHg diagnosed with right heart cath. There is a WHO classification system to categorize the etiologies of pHTN. Our patient above is categorized as group I and III.
Group 1: Pulmonary Arterial Hypertension: idiopathic, inherited, or related to connective tissues diseases
Group 2: pHTN 2/2 LV dysfunction (most common overall)
Group 3: pHTN 2/2 parenchymal lung disease or chronic hypoxia (i.e. COPD, ILD)
Group 4: chronic thromboembolic pHTN (CTEPH)
Group 5: everything else; this is a heterogenous group that encompasses patients with pHTN secondary to hematologic disorders (sickle cell, myeloproliferative disease), systemic diseases (sarcoidosis, vasculitis), and metabolic disease (i.e. glycogen storage disease, thyroid dysfunction)
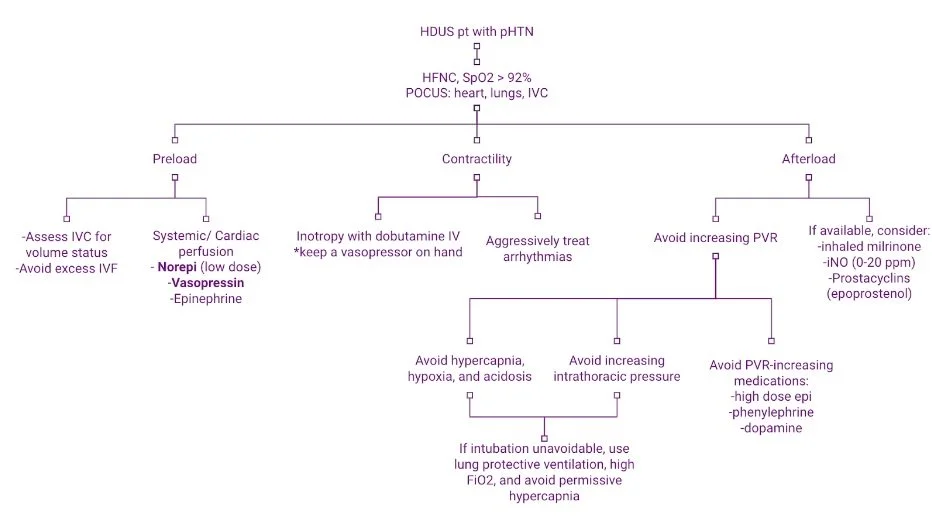
Regardless of the etiology though, pHTN can cause extraordinarily tenuous hemodynamic states when exacerbated by a physiological stressor (such as pneumonia and hypoxia for this patient) and ultimately all roads lead to RV failure. Much of how we learn resuscitation focuses on the LV, but the RV’s hemodynamics are critical to understand. I find it helpful to think about these patient’s physiology by categorizing interventions based on optimizing RV preload, afterload, and contractility/cardiac perfusion.
RV Preload
The RV is very sensitive to alterations in preload. Frank Starling concepts still apply and augmenting preload is important, but unlike the LV, the RV is a low pressure system and very quickly can get overloaded with excess fluid resuscitation. If there is sufficient clinical evidence to suggest hypovolemia, very small fluid boluses (250-500 mL) can be trialed with frequent reassessment with bedside ultrasound. More often than not though, it's probably best to avoid fluids altogether. If there is any evidence at all of volume overload, diuresis should be considered.
If hypotension becomes an issue, reach for vasopressors early. As usual, norepinephrine is a good first line option. Ideally, the vasopressor of choice in pHTN would increase SVR while reducing PVR. The closest thing we have to this is probably vasopressin. Epi at low doses can be considered since it has only modest effect on PVR and provides some inotropy. However, beware of precipitating tachyarrhythmias, which are poorly tolerated in these patients. Pure alpha agonists (i.e. phenylephrine) should be avoided as they will increase PVR.
RV Contractility
RV contractility can be augmented with either milrinone, dobutamine, or epi. Milrinone and dobutamine (to a slightly lesser extent) will also decrease PVR. In the ED setting, dobutamine is likely the safest option. Be aware that both milrinone and dobutamine may decrease SVR, so hypotension should be anticipated and they should be used alongside a pressor. In general, IV milrinone should not be started in the ED as it is more likely to cause hypotension compared to dobutamine, and is renally cleared so may not be the best option in patients with renal failure. Epi will augment contractility and may be considered at lower doses, but is less ideal compared to dobutamine as it will increase PVR.
RV Afterload
This one is tricky in the ED. In an ICU, agents such as epoprostenol (prostacyclins) and inhaled nitric oxide (iNO) may be readily available, but this is often not the case in the ED setting. Inhaled milrinone (2.5-5 mg via nebulizer) can be considered as a quick-and-dirty way of decreasing PVR, but is not the preferred management in ICU settings. If your patient is on a continuous pHTN med like this patient is (treprostinil aka Remodulin), make sure it is not inadvertently discontinued. Beyond that, managing RV afterload has to do with avoiding the following:
Hypoxia
Hypercapnia
Acidosis
Agitation
Increased intrathoracic pressure (i.e. PPV)
Medications that increase PVR (i.e. phenylephrine, high-dose epi)
Managing oxygenation and ventilation can be tricky for these patients since intubation and even NIPPV aren’t great options. The best option is probably HFNC, which can oxygenate well and provides only a modest amount of PEEP. If intubation is starting to seem unavoidable, it is reasonable to trial BIPAP first to preoxygenate. Intubation should be delayed/avoided as much as possible, but if unavoidable, optimize chances of first-pass success in order to limit apneic time. Hemodynamically neutral induction agents should be used and it is a good idea to keep push-dose epi on hand to prevent hypotension with induction.
Hopefully all of the above management should keep your patient afloat until they can get up to an ICU, but if nothing is working and your patient is continuing to decompensate, VA-ECMO should be considered.
Case Close
Our patient is started on HFNC and with improvement in her respiratory status and her O2 sat is maintained >92%. Her blood pressure remains stable initially but later her MAP dips to 57 so she is started on low-dose norepi. Intubation is avoided, and she is admitted to the ICU for respiratory monitoring and further management by her pHTN specialists.
References
Greenwood JC, Winters M. Pulmonary hypertension. In: Tintinalli JE, Ma OJ, Yealy DM, et al., eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 9th ed. McGraw Hill; 2020:(Ch) 58. https://accessmedicine.mhmedical.com/content.aspx?bookid=2353§ionid=219641840
Hoeper MM, Granton J. Intensive care unit management of patients with severe pulmonary hypertension and right heart failure. Am J Respir Crit Care Med. 2011;184(10):1114-1124. https://www.atsjournals.org/doi/10.1164/rccm.201104-0662CI?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub++0pubmed&
Wilcox SR, Kabrhel C, Channick RN. Pulmonary Hypertension and Right Ventricular Failure in Emergency Medicine. Ann Emerg Med. 2015;66(6):619-628. https://www.annemergmed.com/article/S0196-0644(15)01115-4/fulltext