Peripartum Resuscitation
February 2024
Author: Destinee Soubannarath Gwee, MD PGY3
Peer Reviewers: Reena Sheth, MD PGY-3, Michael DeFilippo, DO MICP PGY-4
Faculty Editor: Dr. Anthony Grandelis, MD, Assistant Professor of Obstetrics and Gynecology at Columbia Irving Medical Center and Director of OB/GYN Medical Education at Allen Hospital
The authors of this article have no industry relationships or conflicts of interest to disclose.
Case:
The red phone rings – EMS is bringing in a 32-year-old woman with shortness of breath and hypotension. She is visibly gravid and presumed pregnant. When she arrives in the ED, she looks pale and weak. Her vitals are below:
HR 115
BP 85/50
RR 22
O2 sat 97%
As you’re beginning the interview, the patient loses her pulses. What next?
Begin basic and advanced life support measures (eg, CPR, ACLS)
Establish IV/IO access and administer fluid or blood as needed
Estimate gestational age if unknown
What considerations do we need to make given the patient’s pregnancy?
Overview of the Physiology and Pathophysiology associated with Pregnancy-Related Resuscitation
-Blood volume and cardiac output increase by 30-40% above the non-pregnant state by 28 weeks
Cardiac output increases even further to 50% during labor
Uterine blood flow is up to 20% of cardiac output at term
-Clinical signs of maternal shock manifest only after 40% of maternal blood volume is lost
-Pregnant women are susceptible to hypotension from inferior vena cava (IVC) compression
Significant compression begins at approximately 20 weeks
Chest compressions are also less effective in pregnancy because of IVC compression and decreased venous return
Consider as a cause of hypotension if the fundal height is above the umbilicus
-Enlarged uterus causes elevation of the diaphragm by about 4 cm, and results in a decreased functional residual capacity (FRC) by 20%
Reduced FRC, end expiratory volume, and residual volume result in pregnant patients being less capable of tolerating conditions which require increased oxygen requirements
-Mucosal edema and hyperemia of airway
If intubating, use 1 size smaller ETT
Results in a narrowed airway, increased bleeding and decreased visualization during intubation
Failed intubation rates are 1:250 in pregnancy
-More likely to regurgitate or aspirate given relaxation of the lower esophageal sphincter and increased intra-abdominal pressure from the uterus
What are the likely causes of cardiac arrest in this patient?
Differential Diagnosis for Cardiac Arrest in Pregnancy (Remember ABCDEFGH)
Anesthetics (high spinal, local anesthetic); Accidents (trauma [blood loss; likely cause in our case])
Bleeding (abruption [likely cause in our case, atony, abnormally adherent placentation, coagulopathy)
Cardiovascular (valvular disease, ischemia, dysrhythmia, dissection, congenital cardiac disease)
Drugs (overdose, anaphylaxis, magnesium toxicity)
Embolism
Fever (sepsis)
General (eg, “The Hs and Ts” of ACLS)
Hypertension (pre-eclampsia / eclampsia)
Advanced Cardiac Life Support in Pregnancy
CPR is the same for pregnant patients as it is for non-pregnant patients
Mid-lower sternum hand position
It is okay to use any ACLS medications in pregnancy
It is okay to use defibrillation and cardioversion in pregnancy
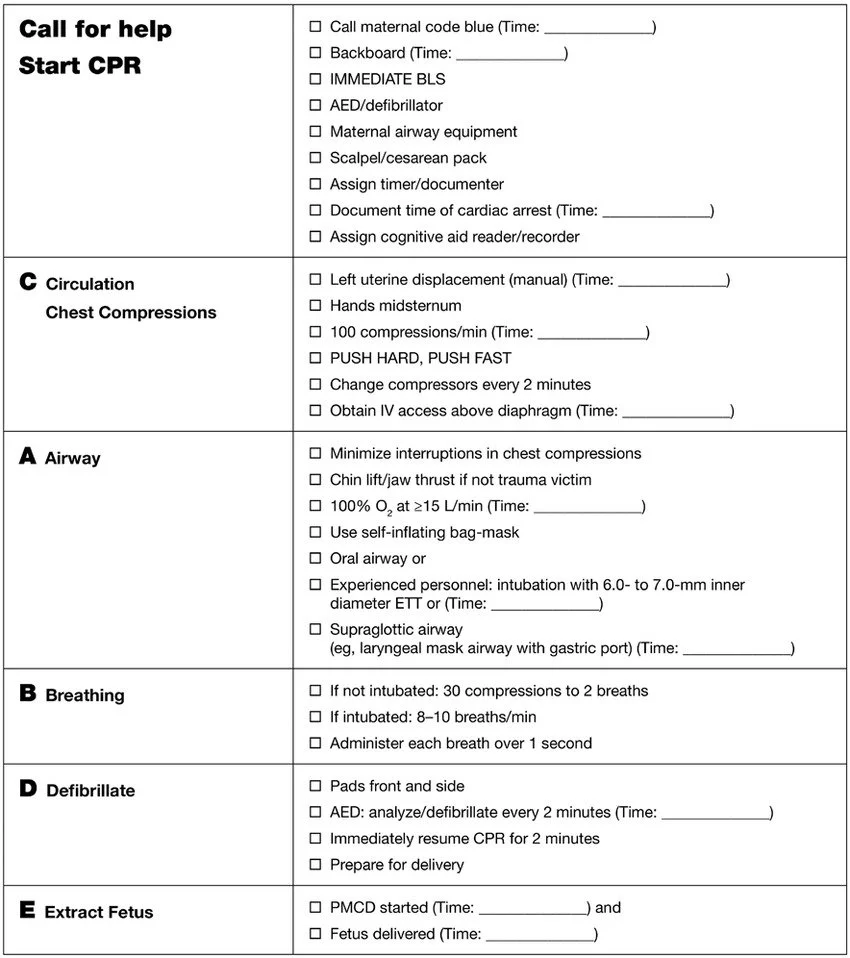
The authors of this post recommend the use of a checklist for maternal cardiac arrest as a cognitive aid during the resuscitation of a pregnant person in cardiac arrest:
Table 1. Checklist of Key Tasks During the First Minutes of In-House Maternal Cardiac Arrest
Source: The Society for Obstetric Anesthesia and Perinatology Consensus Statement on the Management of Cardiac Arrest in Pregnancy. Anesthesia & Analgesia118(5):1003-1016, May 2014.
Procedures for Peripartum Resuscitation: Manual Left Uterine Displacement
With either one or two hands, have someone push or pull the uterus from the right side of the body toward the left side of the body to decrease IVC compression from the gravid uterus.
Jeejeebhoy, Farida & Morrison, Laurie. (2013). Maternal Cardiac Arrest: A Practical and Comprehensive Review. Emergency medicine international. 2013. 274814. 10.1155/2013/274814.
Procedures for Peripartum Resuscitation: Resuscitative Hysterotomy
Previously referred to as the perimortem C-section, resuscitative hysterotomy should only be considered if we think the fetus and uterus are large enough to be causing significant IVC compression (recall, if the fundal height is above the umbilicus).
The traditional model was that the fetus should be >24 weeks for infant viability, but resuscitative hysterotomy is done primarily to prevent maternal mortality, not fetal mortality. Furthermore, saving the mother is the best chance for saving the baby. If the fetus is not >20 weeks (or above the umbilicus if you do not know gestational age), then it is probably not large enough to be causing IVC compression that is contributing to maternal hemodynamics.
Challenging the 4-minute Rule
Both the American College of Obstetrics and Gynecology (ACOG) and the American Heart Association (AHA) currently recommend consideration of resuscitative hysterotomy within the first 4 minutes of cardiac arrest and completing the delivery of the fetus by the 5th minute, allowing a critical 1-minute window for the entire delivery process. This guidance stems from a pivotal case documented by Katz et al in 1986, introducing the '4-minute rule.' Katz and colleagues justified this timeframe by highlighting that adults typically begin experiencing anoxic brain damage within 4 to 6 minutes of a cardiac arrest.
A study published in the Lancet in 2016 by Benson et al challenges this rule. They found that half of maternal/fetal pairs who are delivered by Cesarean birth within 25 minutes survive without injury. The injury free survival rate for both mother and baby has a roughly linear decrease as the time interval from arrest to birth increases.
The study further revealed that only 10% of emergency cesarean sections conducted during maternal cardiac arrest were completed within 1 minute of the initial skin incision. In a prospective cohort study conducted by Alexander et al in 2006, of 37,110 cesarean deliveries, it was found that merely 3,323 of them had incision-to-birth intervals of 3 minutes or less (9%). Of note, these numbers are derived from cesarean deliveries executed by experienced Ob/Gyn specialists in operating room settings.
Considering the context of these findings, it raises doubts about the feasibility for most Emergency Department physicians to complete a resuscitative hysterotomy and then deliver the fetus in less than one minute.
Preparing for the Resuscitative Hysterotomy
For the mother:
If present at your facility, page ObGyn
Assign a team member to continue ACLS if you are going to be performing the hysterotomy
Obtain sterile gloves, scalpel, scissors, gloves, 2 clamps, retractor, laparotomy sponges, and staples
For the baby:
If present at your facility, page neonatal ICU and pediatric EM team
Operationalize a second team to prepare to resuscitate the neonate
Obtain a baby warmer, towels, and ventilatory support supplies
How to Perform the Resuscitative Hysterotomy
Begin with a vertical skin incision from xiphoid process to pubic symphisis
Bluntly dissect the rectus muscles with your fingers
Dissect the peritoneum with fingers or with scissors
Enter the peritoneum bluntly with your fingers
Make a vertical incision at the inferior aspect of the uterus, insert your fingers as a guide, then use scissors to open up the uterus
Deliver the fetus, clamp the cord with two clamps and cut; hand over the fetus to the neonatal resuscitation team
Deliver the placenta
Pack the uterus with sterile towels; bleeding will be minimal given the arrest in circulation
Staple the abdomen closed
Continue with the resuscitation
A video on how to perform a resuscitative hysterotomy by Dr. Sara Gray from Essentials of EMCrit 2018
Case Wrap-Up & Take Home Points
The fundal height is palpated above the umbilicus. A resuscitative hysterotomy was performed which revealed placental abruption. The patient was resuscitated with blood products with return of spontaneous circulation, and the fetus was successfully resuscitated by the neonatal resuscitation team after delivery. Your patient was transferred to the surgical ICU.
Take Home Points
Treat for hypotension even before clinical signs present
Physiology of pregnancy creates unique challenges in resuscitation
Hand placement for CPR is the same as for non-pregnant patients
Consider a broad differential diagnosis, including etiologies unique to pregnancy
Can use the same ACLS medications and electricity in pregnancy
Move the uterus to the left to decreased IVC compression
Resuscitative hysterotomy is only beneficial if the fetus is large enough to be causing IVC compression (above the umbilicus = > 20 weeks)
Resuscitative hysterotomy should be considered early on in resuscitation, however, it seems to have benefit to both mother and baby even if done after the current 4-minute recommendation
References
Bhandari, S. (2015, December 2). Peri-mortem C-section. Core EM. https://coreem.net/core/peri-mortem-c-section/
Munnur U, de Boisblanc B, Suresh MS. Airway problems in pregnancy. Crit Care Med. 2005 Oct;33(10 Suppl):S259-68. Erratum in: Crit Care Med. 2006 Jan;34(1):273. PMID: 16215346.
Lipman S, Cohen S, Einav S, Jeejeebhoy F, et al. Society for Obstetric Anesthesia and Perinatology. The Society for Obstetric Anesthesia and Perinatology consensus statement on the management of cardiac arrest in pregnancy. Anesth Analg. 2014; 118:1003–1016.
Jeejeebhoy, Farida & Morrison, Laurie. (2013). Maternal Cardiac Arrest: A Practical and Comprehensive Review. Emergency medicine international. 2013.
Katz VL, Dotters DJ, Droegemueller W. Perimortem cesarean delivery. Obstet Gynecol. 1986 Oct;68(4):571-6.
Benson MD, Padovano A, Bourjeily G, Zhou Y. Maternal collapse: Challenging the four-minute rule. EBioMedicine. 2016 Apr;6:253-257.
Alexander J.M., Leveno K.J., Hauth J., et al. Fetal injury associated with cesarean delivery. Obstet Gynecol. 2006; 108: 885-890 .
YouTube. (2018). Live Resuscitative Hysterotomy by Dr. Sara Gray: Essentials of EMCrit 2018. YouTube. Retrieved November 31, 2023, from https://www.youtube.com/watch?v=IwDWv2iyAos&ab_channel=HippoEM.
Lipman S, Cohen S, Einav S, et al. The society for obstetric anesthesia and perinatology consensus statement on the management of cardiac arrest in pregnancy. Anesth Analg 2014;118:1003-116
Jeejeebhoy F, Windrim R. Management of cardiac arrest in pregnancy. Best Practice & Research Clinical Obstetrics and Gynaecology 2018; 28:607-618