Hypoxemia and the Blood Gas
January 2024
Author: Lauren Kaplan, MD PGY3
Peer Reviewers: Reena Sheth, MD PGY-3, Shriman Balasubramanian, DO PGY-3, Matthew Villanyi, MD PGY-4
Faculty Editor: Christie Lech, MD, Assistant Professor of Clinical Emergency Medicine at Weill Cornell Medical College, Cornell University
The authors of this article have no industry relationships or conflicts of interest to disclose.
Case:
A 51-year-old female with past medical history notable for having undergone a recent endoscopy presents to the Emergency Department with a chief complaint of “fatigue.” In triage, she is found to have an oxygen saturation of 75% on room air, which improves only to 85% with a non-rebreather mask. Vitals are otherwise unremarkable. You notice perioral cyanosis, but the patient exhibits no other signs of respiratory distress and is speaking in full, clear sentences.
What next?
Overview of Physiology and Pathophysiology
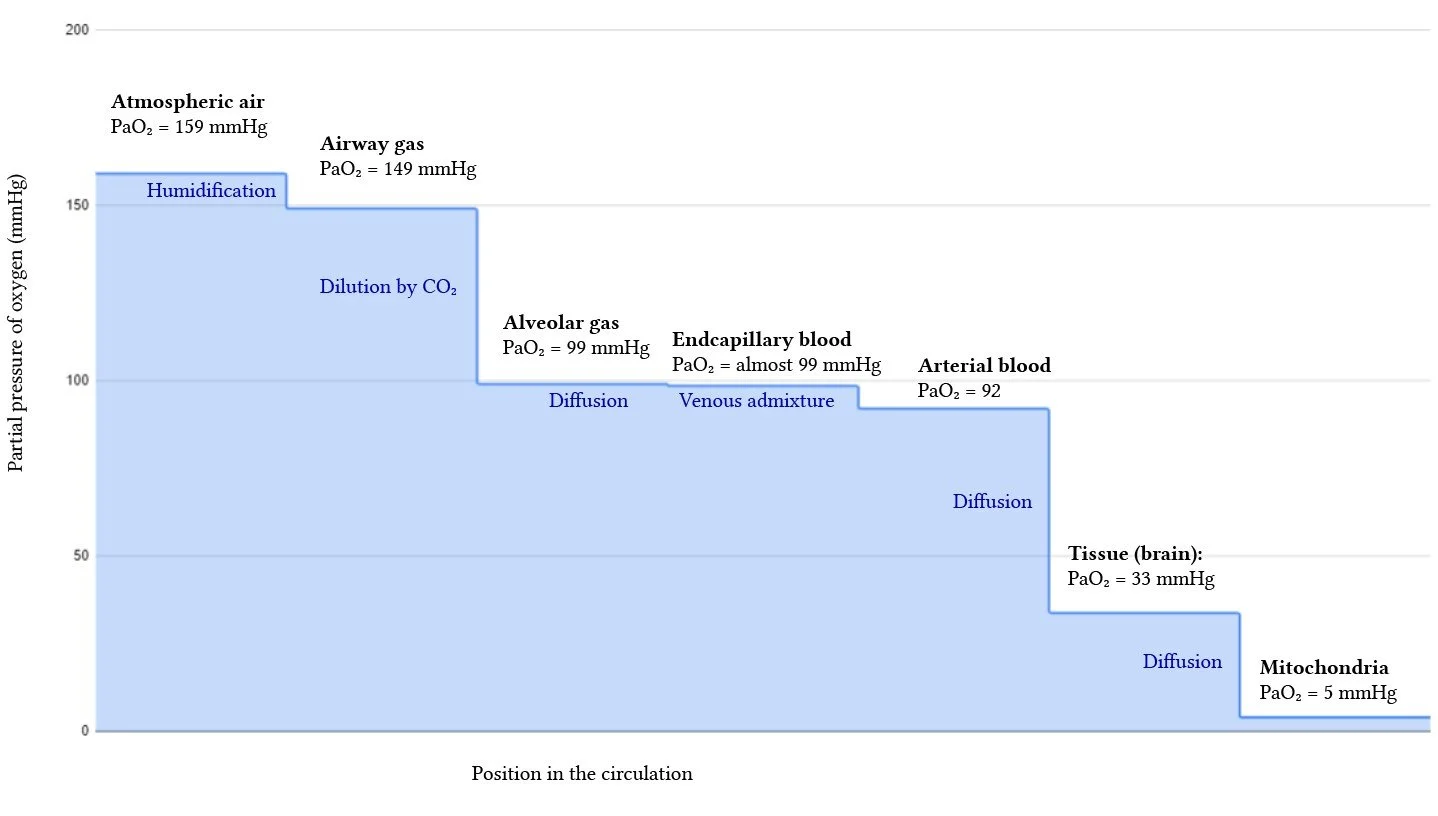
The Oxygen Cascade
Inspired atmospheric air travels through upper and lower airways, to pulmonary alveoli, diffuses across alveolar membranes to pulmonary arteries, and ultimately gets pumped throughout the body to supply vital organs. The amount of inspired oxygen (PaO2) can be affected by factors such as altitude or alterations to FiO2 (fraction of inspired oxygen). The distribution of blood flow to various regions of the lungs is uneven due to gravity: the ratio of ventilation to perfusion (V/Q) thus varies throughout the lungs and can be affected by other disease pathologies. The mechanics of respiration also play a vital role in allowing optimal gas exchange and depend on factors including but not limited to the muscles of inspiration and expiration, lung compliance, and airway resistance.
A small percent of oxygen remains dissolved in arterial blood (~2%) and the remainder gets bound by hemoglobin and transported throughout the rest of the body to supply oxygen to organs and tissues. Oxygen supply thus depends on not only pulmonary factors (PaO2, diffusion, V/Q mismatch) but on hemoglobin carrying capacity and cardiac output.
Source: Yartsev, Alex. (2019). The oxygen cascade. Deranged Physiology. Web
PaO2 = partial pressure of alveolar oxygen
FiO2 = fraction of inspired oxygen (0.21 in room air)
PH20 = water vapor pressure in alveoli (usually 47 mmHg)
Patm = atmospheric pressure (760mmHg at sea level)
PaCO2 = partial pressure of carbon dioxide
Respiratory Quotient = 0.8
Alveolar Gas Equation: PaO2 = (FiO2 x (Patm – PH20)) – (PaCO2/RespQ))
Causes of Hypoxemia (Pulmonary)
Five major mechanisms of hypoxemia include:
Hypoventilation (e.g., decreased respiratory drive, neuromuscular weakness)
VQ mismatch (e.g., COPD/asthma, pulmonary embolus)
Shunt (e.g., bronchus obstruction, intracardiac shunt, pneumonia, pulmonary edema)
Diffusion (e.g., ILD)
Reduced inspired O2 (e.g., high altitude)
Source: Constanzo, Linda S. (2014). Physiology Fifth Edition. Saunders Elsevier.
Monitoring Oxygen
Pulse Oximetry (SpO2):
Pulse oximetry is the easiest and quickest way to assess oxygenation. It estimates the oxygen saturation of hemoglobin by transcutaneous light absorption. Systemic O2 delivery depends on oxygen saturation (~98% of oxygen in blood is bound by hemoglobin).
Source: Constanzo, Linda S. (2014). Physiology Fifth Edition. Saunders Elsevier.
PaO2 can be roughly estimated from %O2 saturation as described in the oxygen-hemoglobin dissociation curve – this will be affected by factors such as PCO2, pH, temperature, and 2,3-DPG.
Pulse oximetry depends on pulsatile blood flow (i.e perfusion). Perfusion index (PI) is the ratio between pulsatile and nonpulsatile blood and can indicate the strength of the pulse arriving at the pulse oximeter. In very low perfusion states, there is not enough pulsatile blood flow to generate a waveform on the pulse oximetry. A poor PI can indicate low cardiac output or vasoconstriction and might be a marker to focus on a patient's perfusion rather than oxygenation in cases of poor pulse oximetry waveform.
Limitations: Pulse oximetry is limited by: low perfusion states (low cardiac output, vasoconstriction, hypothermia), dyshemoglobinemia (assumes that dyshemoglobins such as carboxyhemoglobin and methemoglobin are absent), melanin, nail polish, IV dye administration (e.g., methylene blue), and motion artifact.
Venous Blood Gas:
A venous blood gas (VBG) is a valuable alternative to an arterial blood gas (ABG). Similar to an ABG, it measures dissolved oxygen (PaO2) in venous blood, bicarbonate (HCO3), carbon dioxide (pCO2), venous pH, base excess, lactate, and other electrolytes. VBGs are more convenient and less painful in the ED setting, making it a useful tool in the ED.
Oxygen extraction by tissues is proportional to the degree of CO2 dumping into the blood—therefore the differences in pH between an arterial and venous sample can theoretically be predictable and proportional.
VBGs are clinically useful for screening for and trending hypercarbia (ventilation), obtaining lactate, and establishing acid-base status.
Many studies have investigated the reliability of correlation between venous blood samples and arterial blood samples. Many studies have demonstrated reasonable correlation between pH, pCO2, HCO3, and lactate in certain pathologies (Prasad, Kelly, Bloom). Some studies suggest that at further variance from normal values (i.e., severe shock states) correlation and reliability of VBGs (specifically pH and HCO3) decreases, although one study (Prasad) suggests reasonable correlation in patients with hypotension. Data is also limited in patients with mixed acid-base disorders (Bloom).
Limitations: Reliability is impacted by factors such as tourniquet use or if the specimen is sitting out for an extended amount of time during sample processing.
Arterial Blood Gas:
An arterial blood gas is the historical gold standard for blood gas analysis. In terms of oxygenation, it measures the dissolved oxygen content (PaO2) of arterial blood.
In the ED, there are few indications that may necessitate an ABG. Situations can include very poor arterial waveform and absence of reliable pulse oximetry (e.g., in cases of systemic hypoperfusion or vasoconstriction) or concern for dyshemoglobinemia. When unable to reliably use pulse oximetry due to a poor waveform or low perfusion states, it is likely more prudent to focus on hypoperfusion rather than oxygenation; however, obtaining an ABG can help ascertain true oxygenation status when clinically uncertain.
ABGs can be used to calculate P/F ratio (PaO2/FiO2) to assess oxygenation among ventilated patients, which can be used as an indication for proning in ARDS – however this is unlikely to be applicable in the ED. ABGs are also necessary to calculate an A-a gradient (difference between inspired PO2 and a patient’s PaO2) however this is generally not clinically useful in emergency or critical care.
Limitations: ABGs are painful, expensive, and time-consuming, which make it a poor monitoring tool in the ED. Complications include arterial injury, thrombosis, hematoma, and aneurysm formation among others.
Summary:
Pulse oximetry is used universally for monitoring oxygenation among patients in the ED and critical care setting
Blood gas analysis is used for
Establishing acid-base state
Assessing ventilation function
Measuring lactic acid
While arterial blood gas sampling is the gold standard for blood gas measurements, evidence demonstrates that VBG is a valuable alternative and appropriate for most ED applications
In cases of refractory hypoxemia or unreliable pulse oximetry, ABG can help establish oxygenation status
Case Conclusion:
You obtain an ABG, which shows an extremely high PaO2 (>150 mm). The patient continues to look cyanotic and you notice “chocolate” colored blood. The lab analysis detects methemoglobin in the blood gas sample, confirming your suspicions of methemoglobinemia.
References:
Bloom BM et. al. (2014). The role of venous blood gas in the emergency department: a systematic review and meta-analysis. European Journal of Emergency Medicine (2014)21:81—88.
Constanzo, Linda S. (2014). Physiology Fifth Edition. Saunders Elsevier.
Farkas J. (2023). ABG, VBG, and pulse oximetry. IBCC. Web.
Prasad H et. al. (2023). Correlation and agreement between arterial and venous blood gas analysis in patients with hypotension—an emergency department-based cross-sectional study. International Journal of Emergency Medicine. (2023)16:18.
Kelly, Anne-Maree. (2010). Can venous blood gas analysis replace arterial in emergency medical care. Emergency Medicine Australasia (2010)22, 493-498.
Weingart S & Swaminathan A. (2021). Critical care mailbag: perfusion index. EM:RAP.
Yartsev, Alex. (2019). The oxygen cascade. Deranged Physiology. Web.