Approach to Acute Mitral Regurgitation in the ED
October 2023
Author: Sean Aubuchon MD PGY3
Peer Reviewers: Reena Sheth MD PGY3, Michael DeFilippo DO MICP PGY4
Faculty Editor: Angela Barskaya MD, Assistant Professor of Emergency Medicine and Critical Care at Columbia University Medical Center
Case
A 72-year-old male presents to the emergency department in acute respiratory distress. Their family member notes that the patient has been endorsing chest pain for the past few days. Suddenly about one hour prior to arrival, they began to complain of shortness of breath and worsening of their chest pain.
Initial Vitals:
HR 135 bpm
RR 30
SpO2 86% on room air
BP 110/68
T 36.8 C
Blood Glucose 92
Focused, Point-of-Care Ultrasound: hyperdynamic ejection fraction, diffuse B-lines
ECG: inferior leads with new Q waves and T wave inversions, atrial fibrillation with rapid ventricular response
Introduction
This case demonstrates the classic patient presentation of acute papillary muscle rupture (likely their posterior-medial papillary muscle), due to a subacute occlusive myocardial infarction involving their right coronary artery or posterior descending artery. This leads to acute mitral regurgitation (MR) causing pulmonary edema and eventual cardiogenic shock. Other etiologies include endocarditis with valvular vegetations or chordae tendineae rupture due to myxomatous diseases.
Acute MR contrasts chronic MR because the left side of the heart has not had sufficient time to compensate by increasing left atrial compliance and left ventricular stroke volume. Acutely, this results in decreased cardiac output and increased pulmonary capillary wedge pressure. The diagnosis is one that is extremely important to make within the emergency department as surgical intervention is necessary, but often gets overlooked – especially in patients presenting in only mild shock.
Differential and Diagnosis
While other forms of shock such as distributive or hypovolemic can often be diagnosed through a focused history and physical exam, cardiogenic and obstructive shock often require a more comprehensive workup. The physical exam is not always reliable for diagnosing valvular pathology. For example, presence of a new onset systolic murmur should prompt consideration of MR, but this finding is not sensitive and up to 50% of all acute MR lacks an audible murmur.
Point of care ultrasound has become a mainstay for diagnosing cardiogenic shock in the ED. While most EM clinicians are comfortable identifying pericardial effusions or low ejection fraction on bedside ultrasound, valvular assessment tends to be overlooked.
For this case, you should acquire your usual cardiac views, but pay close attention to the mitral valve. Do you see direct evidence of flail leaflet or ruptured papillary muscle? Regardless, evidence of turbulent or regurgitant flow should be assessed using color flow doppler. This is usually best assessed in the apical 4 or 2-chamber view. Applying color flow doppler over the mitral valve, you should begin to see blue retrograde flow into the LA during systole (Figure 1).
Figure 1. Apical 4-chamber view using color flow doppler depicting retrograde flow from LV to LA.
Image from pocus.org
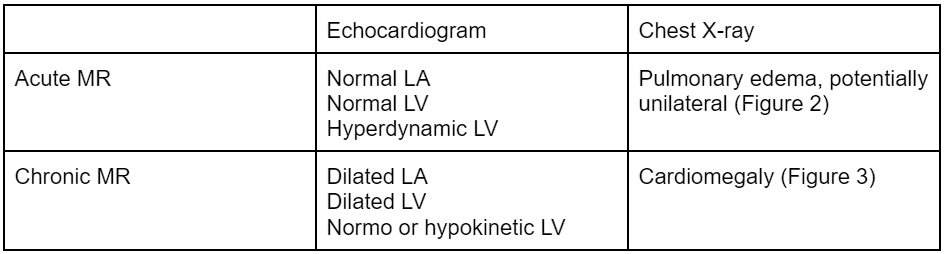
It is also important to distinguish acute mitral regurgitation from chronic mitral regurgitation. For example, if a patient with preexisting moderate or severe chronic mitral regurgitation presents in respiratory distress from sepsis, your initial ultrasound findings of MR may lead you towards an incorrect diagnosis and treatment pathway. Table 1, Figure 2, and Figure 3 highlight some diagnostic differences which can aid in your evaluation.
Table 1. Differences between echocardiogram and chest X-ray findings between acute and chronic MR.
Figure 2. Acute MR with right-sided interstitial edema and normal cardiac silhouette.
Figure 3. Chronic MR with cardiomegaly and clear lungs.
Images from Radiopaedia.com
Initial Medical Management
Acute MR almost always requires surgical intervention – either by cardiothoracic surgery or interventional cardiology. If your institution does not have these services, it is imperative to consider transferring to a tertiary care center early in the clinical course. To get these patients to their definitive care, we must first stabilize using medical management.
Afterload
Increased LV afterload worsens regurgitant flow. To combat this, we must decrease afterload as much as possible without sacrificing end-organ perfusion. This will increase stroke volume, cardiac output, and reduce pulmonary capillary wedge pressure. Medications to consider are high-dose nitroglycerin, nitroprusside, and even dihydropyridine calcium channel blockers such as nicardipine. These medications are usually reserved for patients that primarily have significant pulmonary edema, but still have preserved mean arterial pressures (MAP) or only early signs of cardiogenic shock. Patients in later stages of cardiogenic shock with signs of end-organ dysfunction such as altered mental status or acute kidney injury will likely not tolerate these interventions.
Preload
Measures to reduce preload will not only reduce pulmonary edema but also optimize left ventricular stroke volume. Nitroglycerin or diuresis with a loop diuretic are valid options. In addition, non-invasive positive pressure ventilation (NIPPV) is usually a go-to. Not only will this improve oxygenation, but it will also reduce both preload and afterload.
Heart Rate
Acute MR patients will often present with tachycardia as a compensatory measure to preserve cardiac output. This holds true for patients with atrial fibrillation with rapid ventricular response, such as the patient depicted in our case. In other disease processes, it may be wise to control their heart rate (HR) to improve filling times and improve cardiac output. However, in MR, this is ill advised. The slower the HR, the more time spent in diastole, and the increase in regurgitant flow. Agents with negative chronotropy should be avoided, and providers should tolerate mild tachycardia even in the setting of atrial fibrillation.
Deteriorating or Extremis
Patients presenting with non-perfusing blood pressures, severe respiratory distress, or altered mental status must be managed more aggressively. If NIPPV is not sufficient, have a low threshold for intubation. Inotropes such as epinephrine and dobutamine are preferred. Epinephrine will increase afterload and theoretically worsen regurgitant flow, however, the increase in chronotropy and inotropy will offset this effect. Dobutamine may decrease afterload, so in addition to improving cardiac output, it will also reduce regurgitant flow. Pure afterload agents such as phenylephrine or vasopressin should be avoided. Mechanical circulatory support (MCS) as a bridge to definitive surgical management should be considered for patient’s presenting in extremis that do not immediately improve with medical management (eg, Impella, Extra-corporeal Membrane Oxygenation (ECMO), etc).
Overview of Acute MR
Cardiac output is afterload sensitive – target lowest blood pressure that still maintains organ perfusion; consider nitroglycerin, nitroprusside, nicardipine if MAP allows for adequate perfusion pressure.
Pulmonary edema can be improved with preload reduction; consider nitroglycerin, diuresis, and NIPPV.
Regurgitant flow is inversely related to heart rate; avoid bradycardia.
Severe pulmonary edema may require aggressive respiratory support including NIPPV and intubation.
Cardiogenic shock can be temporized with epinephrine and dobutamine as tolerated.
Medical refractory cardiogenic shock may require MCS as a bridge to intervention so consult specialists early.
References
Augustin, K. (2023, May 26). Acute Valve Disasters – Critical Aortic & Mitral Regurgitation. EMCrit Project. https://emcrit.org/emcrit/valve-disasters-regurg/
Bernard, Deferm, S., & Bertrand, P. B. (2022). Acute valvular emergencies. European Heart Journal. Acute Cardiovascular Care, 11(8), 653–665. https://doi.org/10.1093/ehjacc/zuac086
Bickle, I. (2023, September 3). Mitral valve regurgitation: Radiology reference article. Radiopaedia. https://radiopaedia.org/articles/mitral-valve-regurgitation
Burns B (2017). Valvular emergencies. Cydulka R.K., & Fitch M.T., & Joing S.A., & Wang V.J., & Cline D.M., & Ma O(Eds.), Tintinalli's Emergency Medicine Manual, 8e. McGraw Hill. https://accessemergencymedicine-mhmedical-com.ezproxy.med.cornell.edu/content.aspx?bookid=2158§ionid=162269684
Mitral valve flow analysis with color doppler: Case studies. Point-of-Care Ultrasound Certification Academy. (2022, February 7). https://www.pocus.org/resources/mitral-valve-flow-analysis-with-color-doppler/
Watanabe, N. (2019). Acute mitral regurgitation. Heart, 105(9), 671–677. https://doi.org/10.1136/heartjnl-2018-313373
Zack, J. (2020b, April 9). Acute Valvular Emergencies: Pearls and Pitfalls. emDOCs.net - Emergency Medicine Education. http://www.emdocs.net/acute-valvular-emergencies-pearls-pitfalls/